Children’s charity Action Medical Research is funding new research into progressive familial intrahepatic cholestasis type 3 (PFIC3), a rare severe inherited condition which affects young children like Eva and causes liver disease, often resulting in liver failure.
Rare inherited conditions like PFIC3 can be difficult to diagnose and it took several months to get a diagnosis for Eva. Eva’s mum, Sophie, helped diagnose her daughter’s condition using her training as a biologist and conducted in-depth online research which helped her work out what might be causing her daughter’s symptoms.
“Eva was admitted to hospital when she was 10 days old as she’d had a seizure. She spent most of the first months of her life in hospital and was classed as ‘failing to thrive’. She wasn’t really growing, was distressed, very thin and had constant sickness and diarrhoea. It was so hard to get a diagnosis even though she had so many tests. I was tearing my hair out, so I did a lot of online research and found out about PFIC. I asked doctors to test Eva for this and she was diagnosed when she was just nine months old. The doctors told me that we probably wouldn’t have had a diagnosis when we did if I hadn’t pushed for it,” says Sophie.

Progressive familial intrahepatic cholestasis type 3 is caused by faults in a gene called ABCB4, which provides the instructions to make a protein needed for healthy liver function. In children with PFIC3 the bile, a digestive fluid produced by the liver, lacks an essential component that protects the cells lining the bile ducts (the tubes along which the bile flows from the liver) from its corrosive properties. This means that the bile causes damage and scarring – and eventually the damaged cells stop working, causing liver failure.
Eva was diagnosed with PFIC3 when she was nine months old, and although she was treated early, she has already experienced scarring to her liver and has developed anaemia. Although PFIC3 is a liver disease, it can affect the whole body, including the brain, eyes and growth. The only effective treatment for the condition is a liver transplant, but this is a major operation and has a risk of complications – and there is a shortage of donor livers.
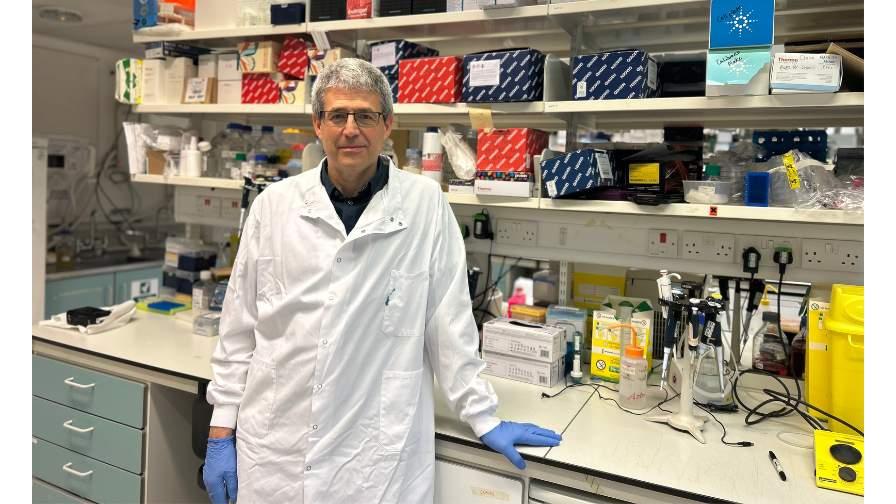
Professor Paul Gissen and the team at the Department of Genetics and Genomic Medicine, UCL Great Ormond Street Institute of Child Health, University College London (UCL), are conducting research into a new gene therapy for children with liver disease caused by faults in the ABCB4 gene. “The research is investigating how to deliver a working copy of the ABCB4 gene, via the bloodstream, into liver cells. This is a novel approach and could be a stepping stone towards setting up a clinical trial for children with PFIC3 which could transform the lives of children with PFIC3 – sparing them from the long waits and complications often associated with liver transplants,” says Professor Gissen.
This research, if successful, could ultimately lead to a safer and better treatment option for children with this life-threatening condition.
Dr Caroline Johnston, Senior Research Manager at Action Medical Research says: “Funding innovative and groundbreaking research into rare disease is an important part of our strategy. 75% of rare diseases affect children and for many of the conditions, there is no effective treatment. This research could lead to a new effective treatment to help children with PFIC3, like Eva.”
To find out more about this and to support this research, please visit: www.action.org.uk/eva.
